NR503 FINAL EXAM STUDY GUIDE ACTUAL 2025/2026 Q&A 100% PASS
Course:
NR 503
Institution:
NR 503
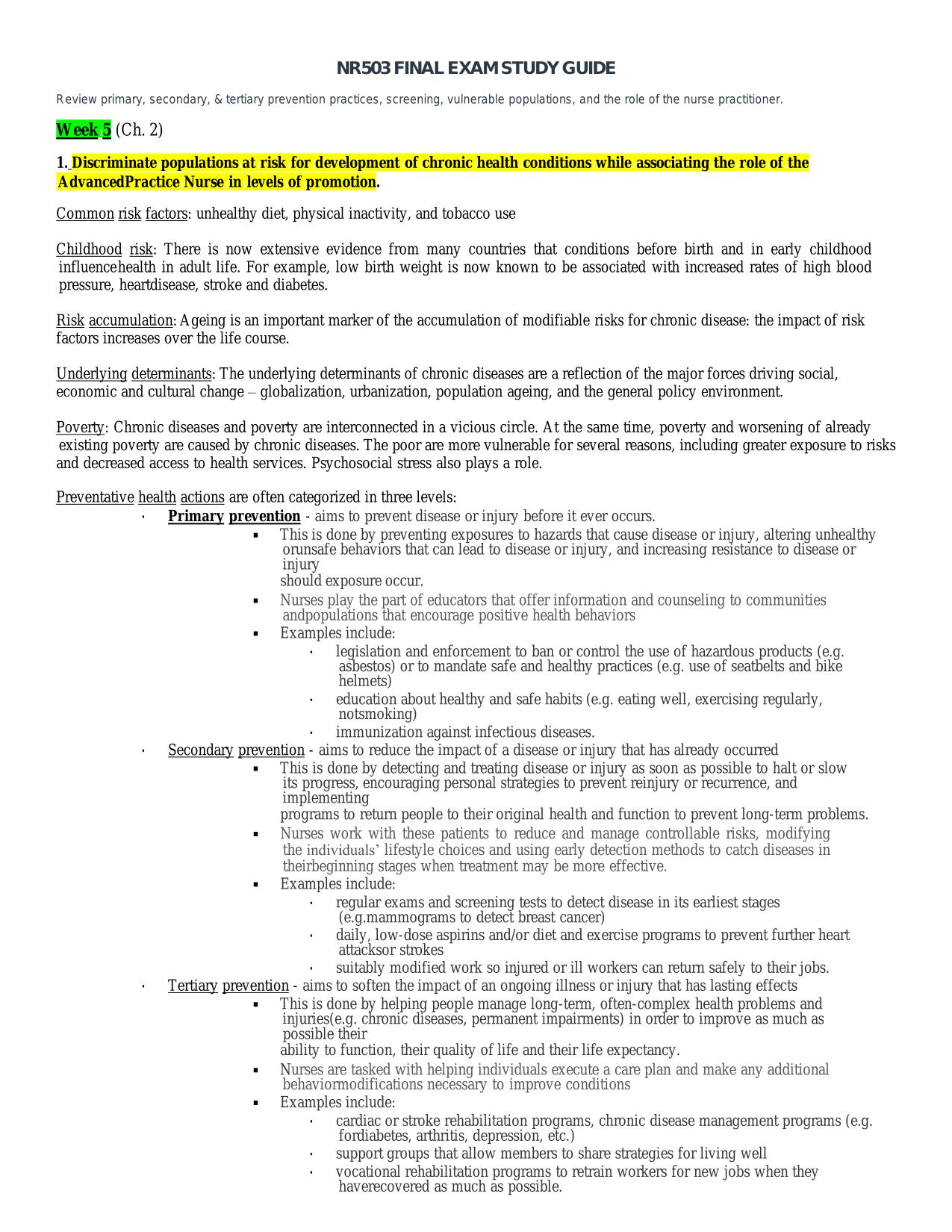
NR503IFINALIEXAMISTUDYIGUIDE Review Iprimary, Isecondary, I&Itertiary Iprevention Ipractices, Iscreening, Ivulnerable Ipopulations, Iand ItheIroleIof ItheInurseIpractitioner. WeekI5I(Ch.I2) 1. DiscriminateIpopulationsIat Irisk IforIdevelopment IofIch...
After purchase, you get:
✅ Instant PDF Download
✅ Verified answer explanations
✅ Refund if not Satisfied
✅ Prepared for 2025/2026 test cycle
Document Information
| Uploaded on: | November 1, 2025 |
| Last updated: | November 1, 2025 |
| Number of pages: | 26 |
| Written in: | 2025/2026 |
| Type: | Exam (elaborations) |
| Contains: | Questions & Answers |
| Tags: | NR503IFINALIEXAMISTUDYIGUIDE Review Iprimary, Isecondary, I&Itertiary Iprevention Ipractices, Iscreening, Ivulnerable Ipopulations, Iand ItheIroleIof ItheInurseIpractitioner. WeekI5I(Ch.I2) 1. DiscriminateIpopulationsIat Irisk IforIdevelopment IofIchronicIhealthIconditionsIwhile Iassociating Ithe IroleIofIthe IAdvancedIPractice INurse Iin Ilevels Iof Ipromotion. CommonIriskIfactors:IunhealthyIdiet,IphysicalIinactivity,Iand Itobacco Iuse Childhood Irisk: IThere Iis Inow Iextensive Ievidence Ifrom Imany Icountries Ithat Iconditions Ibefore Ibirth Iand Iin Iearly Ichildhood IinfluenceIhealth Iin Iadult Ilife. IFor Iexample, Ilow Ibirth Iweight Iis Inow Iknown Ito Ibe Iassociated Iwith Iincreased Irates Iof Ihigh Iblood Ipressure, IheartIdisease, Istroke Iand Idiabetes. Risk Iaccumulation:IAgeing IisIan Iimportant ImarkerIofIthe Iaccumulation IofImodifiable IrisksIforIchronicIdisease: ItheIimpactIofIrisk IfactorsIincreasesIover ItheIlifeIcourse. UnderlyingIdeterminants:ITheIunderlyingIdeterminantsIofIchronicIdiseasesIareIaIreflectionIofItheImajorIforcesIdriving Isocial, Ieconomic IandIculturalIchangeI– Iglobalization,Iurbanization, Ipopulation Iageing,Iand Ithe IgeneralIpolicy Ienvironment. Poverty: IChronicIdiseases Iand Ipoverty IareIinterconnected IinIa Ivicious Icircle. IAt ItheIsame Itime, Ipoverty Iand Iworsening Iof Ialready Iexisting Ipoverty IareIcausedIby Ichronic Idiseases.ITheIpoorIareImoreIvulnerable IforIseveralIreasons, Iincluding IgreaterIexposureIto Irisks Iand Idecreased Iaccess Ito Ihealth Iservices. IPsychosocial Istress IalsoIplays IaIrole. PreventativeIhealth Iactions IareIoftenIcategorized IinIthreeIlevels: • Primary Iprevention I-Iaims Ito Iprevent Idisease Ior Iinjury Ibefore Iit Iever Ioccurs. ▪ ThisIisIdoneIbyIpreventing Iexposures ItoIhazards Ithat IcauseIdisease IorIinjury, IalteringIunhealthy IorIunsafe IbehaviorsIthatIcanIlead Ito IdiseaseIorIinjury, Iand Iincreasing Iresistance Ito IdiseaseIor Iinjury shouldIexposureIoccur |
Seller Information
AdelineJean
User Reviews (0)
Exam (Elaborations)
$9.50
Bundle Deal! Get all 4 docs for just $15.00
Add to Cart
100% satisfaction guarantee
Refund Upon dissatisfaction
Immediately available after purchase
Available in Both online and PDF
$9.50
| 0 sold
Discover More resources
Available in a Bundle
Content Preview
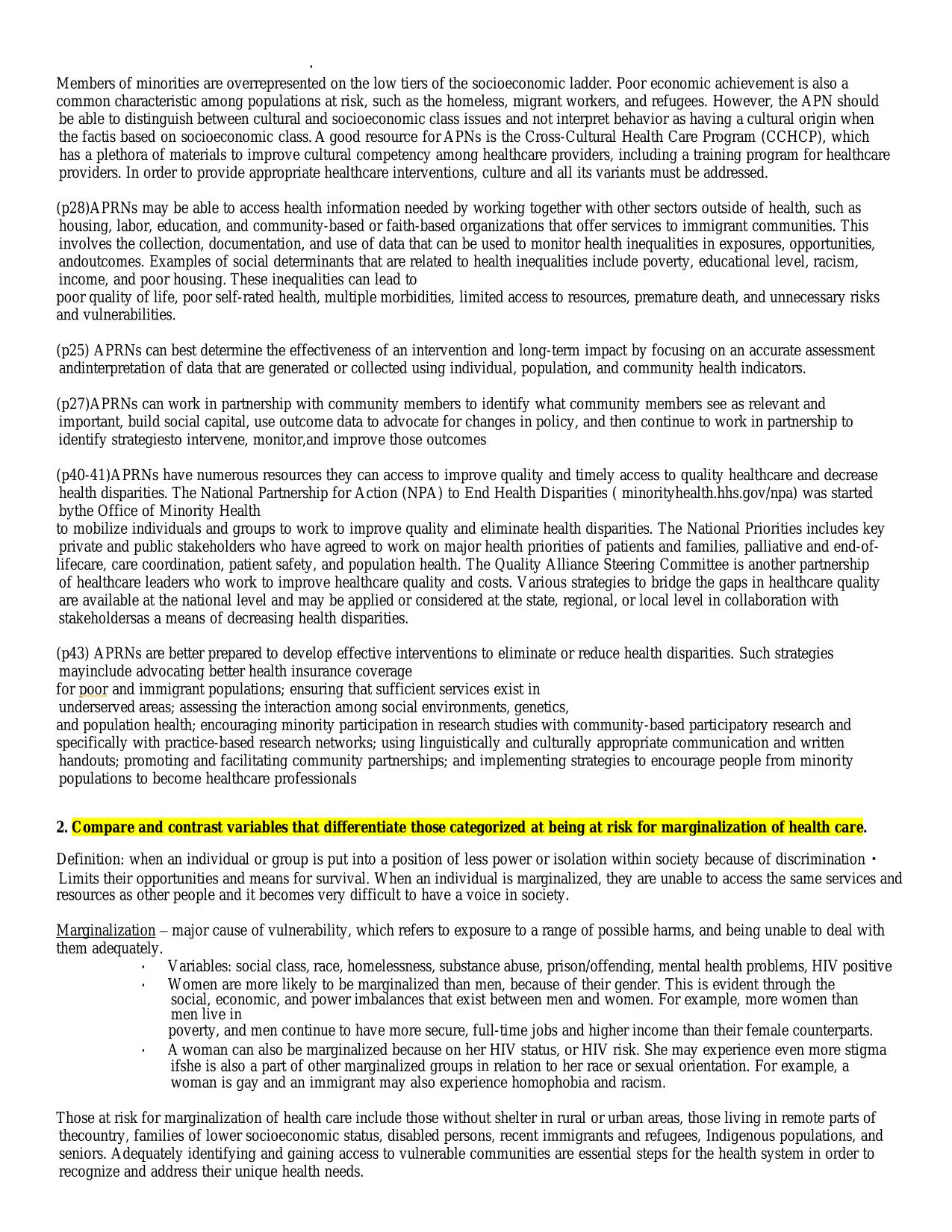
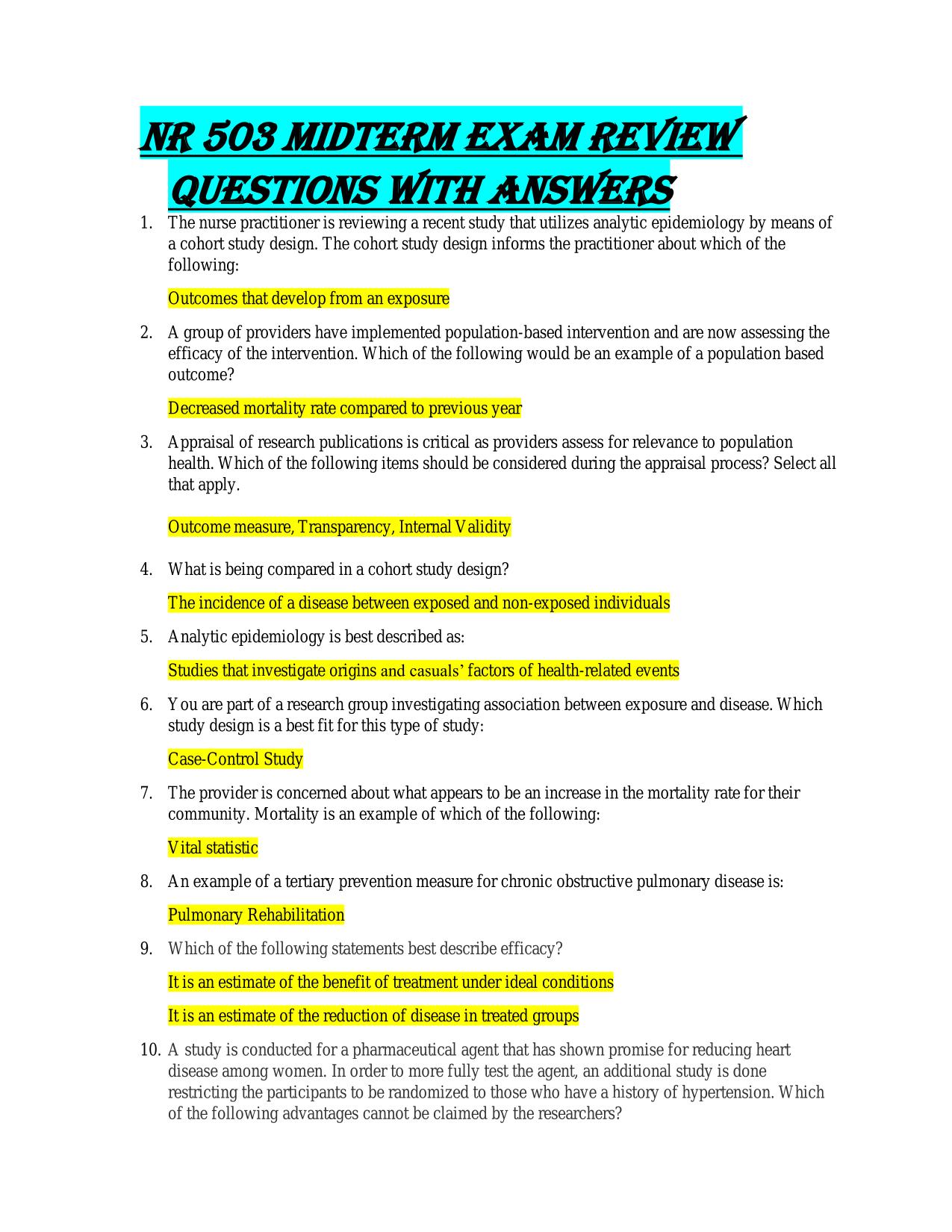
NR503 IFINAL IEXAM ISTUDY IGUIDE Review Iprimary, Isecondary, I& Itertiary Iprevention Ipractices, Iscreening, Ivulnerable Ipopulations, Iand Ithe Irole Iof Ithe Inurse Ipractitioner. Week I5 I(Ch. I2) 1. Discriminate Ipopulations Iat Irisk Ifor Idevelopment Iof Ichronic Ihealth Iconditions Iwhile Iassociating Ithe Irole Iof Ithe IAdvancedIPractice INurse Iin Ilevels Iof Ipromotion. Common Irisk Ifactors: Iunhealthy Idiet, Iphysical Iinactivity, Iand Itobacco Iuse Childhood Irisk: IThere Iis Inow Iextensive Ievidence Ifrom Imany Icountries Ithat Iconditions Ibefore Ibirth Iand Iin Iearly Ichildhood Iinfluence Ihealth Iin Iadult Ilife. IFor Iexample, Ilow Ibirth Iweight Iis Inow Iknown Ito Ibe Iassociated Iwith Iincreased Irates Iof Ihigh Iblood Ipressure, IheartIdisease, Istroke Iand Idiabetes. Risk Iaccumulation: IAgeing Iis Ian Iimportant Imarker Iof Ithe Iaccumulation Iof Imodifiable Irisks Ifor Ichronic Idisease: Ithe Iimpact Iof Irisk Ifactors Iincreases Iover Ithe Ilife Icourse. Underlying Ideterminants: IThe Iunderlying Ideterminants Iof Ichronic Idiseases Iare Ia Ireflection Iof Ithe Imajor Iforces Idriving Isocial, Ieconomic Iand Icultural Ichange I– Iglobalization, Iurbanization, Ipopulation Iageing, Iand Ithe Igeneral Ipolicy Ienvironment. Poverty: IChronic Idiseases Iand Ipoverty Iare Iinterconnected Iin Ia Ivicious Icircle. IAt Ithe Isame Itime, Ipoverty Iand Iworsening Iof Ialready Iexisting Ipoverty Iare Icaused Iby Ichronic Idiseases. IThe Ipoor Iare Imore Ivulnerable Ifor Iseveral Ireasons, Iincluding Igreater Iexposure Ito Irisks Iand Idecreased Iaccess Ito Ihealth Iservices. IPsychosocial Istress Ialso Iplays Ia Irole. Preventative Ihealth Iactions Iare Ioften Icategorized Iin Ithree Ilevels: • Primary Iprevention I- Iaims Ito Iprevent Idisease Ior Iinjury Ibefore Iit Iever Ioccurs. ▪ This Iis Idone Iby Ipreventing Iexposures Ito Ihazards Ithat Icause Idisease Ior Iinjury, Ialtering Iunhealthy IorIunsafe Ibehaviors Ithat Ican Ilead Ito Idisease Ior Iinjury, Iand Iincreasing Iresistance Ito Idisease Ior Iinjury should Iexposure Ioccur. ▪ Nurses Iplay Ithe Ipart Iof Ieducators Ithat Ioffer Iinformation Iand Icounseling Ito Icommunities IandIpopulations Ithat Iencourage Ipositive Ihealth Ibehaviors ▪ Examples Iinclude: • legislation Iand Ienforcement Ito Iban Ior Icontrol Ithe Iuse Iof Ihazardous Iproducts I(e.g. Iasbestos) Ior Ito Imandate Isafe Iand Ihealthy Ipractices I(e.g. Iuse Iof Iseatbelts Iand Ibike Ihelmets) • education Iabout Ihealthy Iand Isafe Ihabits I(e.g. Ieating Iwell, Iexercising Iregularly, InotIsmoking) • immunization Iagainst Iinfectious Idiseases. • Secondary Iprevention I- Iaims Ito Ireduce Ithe Iimpact Iof Ia Idisease Ior Iinjury Ithat Ihas Ialready Ioccurred ▪ This Iis Idone Iby Idetecting Iand Itreating Idisease Ior Iinjury Ias Isoon Ias Ipossible Ito Ihalt Ior Islow Iits Iprogress, Iencouraging Ipersonal Istrategies Ito Iprevent Ireinjury Ior Irecurrence, Iand Iimplementing programs Ito Ireturn Ipeople Ito Itheir Ioriginal Ihealth Iand Ifunction Ito Iprevent Ilong-term Iproblems. ▪ Nurses Iwork Iwith Ithese Ipatients Ito Ireduce Iand Imanage Icontrollable Irisks, Imodifying Ithe Iindividuals’ Ilifestyle Ichoices Iand Iusing Iearly Idetection Imethods Ito Icatch Idiseases Iin ItheirIbeginning Istages Iwhen Itreatment Imay Ibe Imore Ieffective. ▪ Examples Iinclude: • regular Iexams Iand Iscreening Itests Ito Idetect Idisease Iin Iits Iearliest Istages I(e.g.Imammograms Ito Idetect Ibreast Icancer) • daily, Ilow-dose Iaspirins Iand/or Idiet Iand Iexercise Iprograms Ito Iprevent Ifurther Iheart IattacksIor Istrokes • suitably Imodified Iwork Iso Iinjured Ior Iill Iworkers Ican Ireturn Isafely Ito Itheir Ijobs. • Tertiary Iprevention I- Iaims Ito Isoften Ithe Iimpact Iof Ian Iongoing Iillness Ior Iinjury Ithat Ihas Ilasting Ieffects ▪ This Iis Idone Iby Ihelping Ipeople Imanage Ilong-term, Ioften-complex Ihealth Iproblems Iand IinjuriesI(e.g. Ichronic Idiseases, Ipermanent Iimpairments) Iin Iorder Ito Iimprove Ias Imuch Ias Ipossible Itheir ability Ito Ifunction, Itheir Iquality Iof Ilife Iand Itheir Ilife Iexpectancy. ▪ Nurses Iare Itasked Iwith Ihelping Iindividuals Iexecute Ia Icare Iplan Iand Imake Iany Iadditional IbehaviorImodifications Inecessary Ito Iimprove Iconditions ▪ Examples Iinclude: • cardiac Ior Istroke Irehabilitation Iprograms, Ichronic Idisease Imanagement Iprograms I(e.g. IforIdiabetes, Iarthritis, Idepression, Ietc.) • support Igroups Ithat Iallow Imembers Ito Ishare Istrategies Ifor Iliving Iwell • vocational Irehabilitation Iprograms Ito Iretrain Iworkers Ifor Inew Ijobs Iwhen Ithey IhaveIrecovered Ias Imuch Ias Ipossible. • Members Iof Iminorities Iare Ioverrepresented Ion Ithe Ilow Itiers Iof Ithe Isocioeconomic Iladder. IPoor Ieconomic Iachievement Iis Ialso Ia common Icharacteristic Iamong Ipopulations Iat Irisk, Isuch Ias Ithe Ihomeless, Imigrant Iworkers, Iand Irefugees. IHowever, Ithe IAPN Ishould Ibe Iable Ito Idistinguish Ibetween Icultural Iand Isocioeconomic Iclass Iissues Iand Inot Iinterpret Ibehavior Ias Ihaving Ia Icultural Iorigin Iwhen Ithe IfactIis Ibased I on Isocioeconomic Iclass. IA Igood Iresource Ifor IAPNs Iis Ithe ICross-Cultural IHealth ICare IProgram I(CCHCP), Iwhich I has Ia Iplethora Iof Imaterials Ito Iimprove Icultural Icompetency Iamong Ihealthcare Iproviders, Iincluding Ia Itraining Iprogram Ifor Ihealthcare Iproviders. IIn Iorder Ito Iprovide Iappropriate Ihealthcare Iinterventions, Iculture Iand Iall Iits Ivariants Imust Ibe Iaddressed. (p28)APRNs Imay Ibe Iable Ito Iaccess Ihealth Iinformation Ineeded Iby Iworking Itogether Iwith Iother Isectors Ioutside Iof Ihealth, Isuch Ias Ihousing, Ilabor, Ieducation, Iand Icommunity-based Ior Ifaith-based Iorganizations Ithat Ioffer Iservices Ito Iimmigrant Icommunities. IThis Iinvolves Ithe Icollection, Idocumentation, Iand Iuse Iof Idata Ithat Ican Ibe Iused Ito Imonitor Ihealth Iinequalities Iin Iexposures, Iopportunities, IandIoutcomes. IExamples Iof Isocial Ideterminants Ithat Iare Irelated Ito Ihealth Iinequalities Iinclude Ipoverty, Ieducational Ilevel, Iracism, Iincome, Iand Ipoor Ihousing. IThese Iinequalities Ican Ilead Ito poor Iquality Iof Ilife, Ipoor Iself-rated Ihealth, Imultiple Imorbidities, Ilimited Iaccess Ito Iresources, Ipremature Ideath, Iand Iunnecessary Irisks Iand Ivulnerabilities. (p25) IAPRNs Ican Ibest Idetermine Ithe Ieffectiveness Iof Ian Iintervention Iand Ilong-term Iimpact Iby Ifocusing Ion Ian Iaccurate Iassessment IandIinterpretation Iof Idata Ithat Iare Igenerated Ior Icollected Iusing Iindividual, Ipopulation, Iand Icommunity Ihealth Iindicators. (p27)APRNs Ican Iwork Iin Ipartnership Iwith Icommunity Imembers Ito Iidentify Iwhat Icommunity Imembers Isee Ias Irelevant Iand Iimportant, Ibuild Isocial Icapital, Iuse Ioutcome Idata Ito Iadvocate Ifor Ichanges Iin Ipolicy, Iand Ithen Icontinue Ito Iwork Iin Ipartnership Ito Iidentify IstrategiesIto Iintervene, Imonitor,and Iimprove Ithose Ioutcomes (p40-41)APRNs Ihave Inumerous Iresources Ithey Ican Iaccess Ito Iimprove Iquality Iand Itimely Iaccess Ito Iquality Ihealthcare Iand Idecrease Ihealth Idisparities. IThe INational IPartnership Ifor IAction I(NPA) Ito IEnd IHealth IDisparities I( Iminorityhealth.hhs.gov/npa) Iwas Istarted IbyIthe IOffice Iof IMinority IHealth to Imobilize Iindividuals Iand Igroups Ito Iwork Ito Iimprove Iquality Iand Ieliminate Ihealth Idisparities. IThe INational IPriorities Iincludes Ikey Iprivate Iand Ipublic Istakeholders Iwho Ihave Iagreed Ito Iwork Ion Imajor Ihealth Ipriorities Iof Ipatients Iand Ifamilies, Ipalliative Iand Iend-oflifeIcare, Icare Icoordination, Ipatient Isafety, Iand Ipopulation Ihealth. IThe IQuality IAlliance ISteering ICommittee Iis Ianother Ipartnership Iof Ihealthcare Ileaders Iwho Iwork Ito Iimprove Ihealthcare Iquality Iand Icosts. IVarious Istrategies Ito Ibridge Ithe Igaps Iin Ihealthcare Iquality Iare Iavailable Iat Ithe Inational Ilevel Iand Imay Ibe Iapplied Ior Iconsidered Iat Ithe Istate, Iregional, Ior Ilocal Ilevel Iin Icollaboration Iwith IstakeholdersIas Ia Imeans Iof Idecreasing Ihealth Idisparities. (p43) IAPRNs Iare Ibetter Iprepared Ito Idevelop Ieffective Iinterventions Ito Ieliminate Ior Ireduce Ihealth Idisparities. ISuch Istrategies ImayIinclude Iadvocating Ibetter Ihealth Iinsurance Icoverage for Ipoor Iand Iimmigrant Ipopulations; Iensuring Ithat Isufficient Iservices Iexist Iin Iunderserved Iareas; Iassessing Ithe Iinteraction Iamong Isocial Ienvironments, Igenetics, and Ipopulation Ihealth; Iencouraging Iminority Iparticipation Iin Iresearch Istudies Iwith Icommunity-based Iparticipatory Iresearch Iand Ispecifically Iwith Ipractice-based Iresearch Inetworks; Iusing Ilinguistically Iand Iculturally Iappropriate Icommunication Iand Iwritten Ihandouts; Ipromoting Iand Ifacilitating Icommunity Ipartnerships; Iand Iimplementing Istrategies Ito Iencourage Ipeople Ifrom Iminority Ipopulations Ito Ibecome Ihealthcare Iprofessionals 2. Compare Iand Icontrast Ivariables Ithat Idifferentiate Ithose Icategorized Iat Ibeing Iat Irisk Ifor Imarginalization Iof Ihealth Icare. Definition: Iwhen Ian Iindividual Ior Igroup Iis Iput Iinto Ia Iposition Iof Iless Ipower Ior Iisolation Iwithin Isociety Ibecause Iof Idiscrimination I ILimits Itheir Iopportunities Iand Imeans Ifor Isurvival. IWhen Ian Iindividual Iis Imarginalized, Ithey Iare Iunable Ito Iaccess Ithe Isame Iservices Iand Iresources Ias Iother Ipeople Iand Iit Ibecomes Ivery Idifficult Ito Ihave Ia Ivoice Iin Isociety. Marginalization I– Imajor Icause Iof Ivulnerability, Iwhich Irefers Ito Iexposure Ito Ia Irange Iof Ipossible Iharms, Iand Ibeing Iunable Ito Ideal Iwith Ithem Iadequately. • Variables: Isocial Iclass, Irace, Ihomelessness, Isubstance Iabuse, Iprison/offending, Imental Ihealth Iproblems, IHIV Ipositive • Women Iare Imore Ilikely Ito Ibe Imarginalized Ithan Imen, Ibecause Iof Itheir Igender. IThis Iis Ievident Ithrough Ithe Isocial, Ieconomic, Iand Ipower Iimbalances Ithat Iexist Ibetween Imen Iand Iwomen. IFor Iexample, Imore Iwomen Ithan Imen Ilive Iin poverty, Iand Imen Icontinue Ito Ihave Imore Isecure, Ifull-time Ijobs Iand Ihigher Iincome Ithan Itheir Ifemale Icounterparts. • A Iwoman Ican Ialso Ibe Imarginalized Ibecause Ion Iher IHIV Istatus, Ior IHIV Irisk. IShe Imay Iexperience Ieven Imore Istigma IifIshe Iis Ialso Ia Ipart Iof Iother Imarginalized Igroups Iin Irelation Ito Iher Irace Ior Isexual Iorientation. IFor Iexample, Ia Iwoman Iis Igay Iand Ian Iimmigrant Imay Ialso Iexperience Ihomophobia Iand Iracism. Those Iat Irisk Ifor Imarginalization Iof Ihealth Icare Iinclude Ithose Iwithout Ishelter Iin Irural Ior Iurban Iareas, Ithose Iliving Iin Iremote Iparts Iof ItheIcountry, Ifamilies Iof Ilower Isocioeconomic Istatus, Idisabled Ipersons, Irecent Iimmigrants Iand Irefugees, IIndigenous Ipopulations, Iand Iseniors. IAdequately Iidentifying Iand Igaining Iaccess Ito Ivulnerable Icommunities Iare Iessential Isteps Ifor Ithe Ihealth Isystem Iin Iorder Ito Irecognize Iand Iaddress Itheir Iunique Ihealth Ineeds. Four Idimensions Ithat Icapture Ithe Iprincipal Ideterminants Iof Ihealth Imarginalization: Iresidential Iinstability, Imaterial Ideprivation, Iethnic Iconcentration, Iand Idependency. (FYI: II Icouldn’t Ifind Ithis Iinformation Iin Ithe Itext Ibut II Ifound Iit Ihere Ihttps://ubcmj.med.ubc.ca/marginalization-inhealth/)I(online Ilesson Iwk I5) ISingletone Iand IKrause I(2009) Ihave Iidentified Ithe Iconfounding Ivariables Ithat Iresult Iin Isubpar Ihealth communication. IThese Iinclude Ilow Ihealth Iliteracy, Icultural Ibarriers, Iand Ilow IEnglish Iproficiency. IThe Ihealthcare Isystem Iis Ioften Iconfusing Ifor Iindividuals Iwho Iare Iproficient Iin IEnglish Ibut Iare Inot Ifamiliar Iwith Ihealthcare Iknowledge Iand Iterminology. IOne Ican Iimagine Ithe Isynergistic Ieffect Iof Ihaving Ilow Ihealth Iliteracy Iin Iaddition Ito Ihaving Iinadequate IEnglish Iskills. IThe Iconfluence Ican Ihinder Ioptimal Iutilization Iof Ithe Ihealthcare Isystem. (p28)Social Ideterminants Iof Ihealth Iand Iinequalities Idata Iare Iareas Ithat IAPRNs can Ialso Iuse Ito Iinform Iand Iguide Itheir Ipractice Ito Idevelop Isocioculturally IappropriateIinterventions. ISocial Ideterminants Ithat Ilead Ito Ihealth Iinequalities Iare recognized Isituations Irelated Ito Iwhere Ipeople Iare Iborn, Igrow Iup, Iwork, Ilive, and Ithe Isystems Iof Icare Iavailable Ito Ithem Ito Ideal Iwith Iillness Iand Idisease….. IExamples Iof Isocial Ideterminants Ithat Iare Irelated Ito Ihealth Iinequalities Iinclude Ipoverty, Ieducational Ilevel, Iracism, Iincome, Iand Ipoor Ihousing. IThese Iinequalities Ican Ilead Ito poor Iquality Iof Ilife, Ipoor Iself-rated Ihealth, Imultiple Imorbidities, Ilimited Iaccess Ito Iresources, Ipremature Ideath, Iand Iunnecessary Irisks Iand Ivulnerabilities. (p37) IDisparities/inequity Ito Ibe Iassessed Iby Ithe Ifollowing: • Race/ethnicity • Gender • Socioeconomic Istatus • Disability Istatus • LGBT Istatus • Geography (p40) IIt Iis Iwidely Irecognized Inow Ithat Ithe Isocial Ideterminants Iof health, Isuch Ias Ihousing, Ieducation, Iaccess Ito Ipublic Itransportation, Iaccess Ito Isafe Iwater, Iaccess Ito Ifresh Ifood, Iand Ithe Ibuilt Ienvironment, Iare Iall Irelated Ito Ia Ipopulation’s Ihealth. IIn Iaddition Ito Iethnicity, Iother Icharacteristics Ialso IcontributeIto Ithe Ipresence Iof Idisparities Ior Ithe Iachievement Iof Igood Ihealth Isuch Ias gender, Isexual Iorientation, Igeographic Ilocation, Iworking Ienvironment, Icognitive,Isensory, Ior Iphysical Idisability, Iand Isocioeconomic Istatus. 3. How Idoes Iculture Iinfluence Ithe Idecisions Ia Iprovider Imay Imake Iwhen Iselecting Ian Iintervention? Learning Iabout Ione’s Iculture Iand Iassessing Iepidemiological Ipatterns Iof Ihealth Iand Iillness Iacross Ithe Ilife Ispan Ifacilitates Ithe Inurse Ipractitioner's Iability Ito Ifocus Ion Ihealth Iinitiatives Iand Iformulate Iplans Iof Icare Ileading Ito Ibehavioral Ichange Iand Isustainable Iquality Ihealth Iand Ilifestyle Ioutcomes. IReligion, Iculture, Ibeliefs, Iand Iethnic Icustoms Ican Iinfluence Ihow Ipts Iunderstand Ihealth Iconcepts, Ihow Ithey Itake Icare Iof Itheir Ihealth, Iand Ihow Ithey Imake Idecisions Irelated Ito Itheir Ihealth. IWithout Iproper Itraining, Iclinicians Imay Ideliver Imedical Iadvice Iwithout Iunderstanding Ihow Ihealth Ibeliefs Iand Icultural Ipractices Iinfluence Ithe Iway Ithat Iadvice Iis Ireceived. IAsking IaboutIpts’s Ireligions, Icultures, Iand Iethnic Icustoms Ican Ihelp Iclinicians Iengage Ipts Iso Ithat, Itogether, Ithey Ican Idevise Itreatment Iplans Ithat Iare Iconsistent Iwith Ithe Ipt’s Ivalues. Several Imodels Ihave Iemerged Ito Iassist Ihealthcare Iproviders Ito Imeet Ithe Ichallenge Iof Iproviding Iculturally Irelevant Icare. ICampinhaIBacote I(2002) Iviews Icultural Icompetence Ias Ian Iongoing Ilearning Iprocess Ias Ithe Iproviders Icontinuously Istrive Ito Iachieve Ithe Ibest Ioutcomes Ifor Ipatients, Ifamilies, Iand Ipopulations. Culture Iis, I"the Ipractices, Ibeliefs, Ivalues, Iand Inorms Iwhich Ican Ibe Ilearned Ior Ishared, Iand Iwhich Iguide Ithe Iactions Iand Idecisions Iof Ieach Iperson Iin Ithe Igroup”. Health Iand Idisease Idenotes Ican Ivary Ifrom Iculture Ito Iculture. ITherefore, Ithere Iis Ia Iwide Ispectrum Iof Iwhat Iare Iconsidered Iappropriate Iinterventions. IThus, Iculture Iinfluences Ithe Idecisions Ia Iprovider Imay Imake Iwhen Iselecting Ian Iintervention Ibased Ion Ithe Icultures' Iperceptions Iof Idisease Icausation, Isymptomatology, Iand Ipathology. Care Iis Iprovided Iwith Isensitivity Iand Iis Ibased Ion Ithe Icultural Iuniqueness Iof Iclients. although Icultures Idiffer, Ithey Iall Ihave Ithe Isame Ibasic Iorganizing Ifactors Ithat Imust Ibe Iassessed Iin Iorder Ito Iprovide Icare Ifor Iculturally Idiverse Ipatients. IThese Ifactors Iinclude. IAlthough Icultures Idiffer, Ithey Iall Ihave Ithe Isame Ibasic Iorganizing Ifactors Ithat Imust Ibe IassessedIin Iorder Ito Iprovide Icare Ifor Iculturally Idiverse Ipatients. IThese Ifactors Iinclude • communication I(verbal Iand Inonverbal); • • • • • personal Ispace; social Iorganization; time Iperception; environmental Icontrol; Iand biological Ivariations. Several Imodels Ihave Iemerged Ito Iassist Ihealthcare Iproviders Ito Imeet Ithe Ichallenge Iof Iproviding Iculturally Irelevant Icare. Macro-scale Iinfluences: IBroad Iunderstandings Iof Iillness, Isuffering Iand Ihealing, ISocial Iroles Iand Ithe Ibureaucratic Iand Ieconomic Icontext Iof Ihealth Icare Iservices Micro-scale Iinfluences: IFace-to-face Iinteraction Iat Ifront-lines, ISuccessful Iand Ifailed Icommunication (week I5 Ilesson) IThe Ivery Iessence Iof Iwhat Ihealth Iand Idisease Idenotes Ican Ivary Ifrom Iculture Ito Iculture. ITherefore, Ithere Iis Ia Iwide Ispectrum Iof Iwhat Iare Iconsidered Iappropriate Iinterventions, Iwhich Imay Inot Ibe Icompatible Iwith IWestern Imedicine. IBased Ion Ithe Icultures' Iperceptions Iof Idisease Icausation, Isymptomatology, Iand Ipathology, Iappropriate Iinterventions Imay Idiverge Ifrom IWestern Imedicine's Iapproach I(Gesler I& IKearns, I2002). IThe Itextbook Iprovides Imany Iexamples Iof Ithe Ibeliefs Iof Idirect Icultures Iand Ithe IinfluenceIthey Iplay Iin Ihealthcare. IThere Iare Isome Ilong-standing Ihealth Idisparities Iin Iminorities. IMinority Ihealth Iis Ioften Iviewed Ias Ia Ivariant IformIof IAnglo-Protestant Iculture, Iwith Ithe Iscientific Ifoundation Iand Ithe Iprinciples Iof Icause Iand Ieffect Ias Ithe Ibasis Iof Iour Ihealthcare. Cultural Icompetence Iin Inursing Iconsists Iof Ifour Iprinciples. • • • • Care Iis Idesigned Ifor Ithe Ispecific Iclient. Care Iis Ibased Ion Ithe Iuniqueness Iof Ithe Iperson's Iculture Iand Iincludes Icultural Inorms Iand Ivalues. Care Iincludes Iself-employment Istrategies Ito Ifacilitate Iclient Idecision Imaking Ito Iimprove Ihealth Ibehaviors. Care Iis Iprovided Iwith Isensitivity Iand Iis Ibased Ion Ithe Icultural Iuniqueness Iof Iclients. 4. Explain Ihow Iculture Iimpacts Iprovider Iattitudes? I Does Iit? I How Iwill Iyou Iassess Iyour Iown Iattitudes Iabout IvariousIcultures/races/groups? Bias Ican Ioccur. IPatients Iof Icolor Imay Ibe Ikept Iwaiting Ilonger Ifor Iassessment Ior Itreatment Ithan Itheir IWhite Icounterparts, Ior Iproviders Imay Ispend Imore Itime Iwith IWhite Ipatients Ithan Iwith Ipatients Iof Icolor. IRacial/ethnic Ibias Iin Iattitudes, Isuch Ias Ifeeling Ithat IWhite IpeopleIare Inicer Ithan IBlack Ipeople, Iwhether Iconscious Ior Inot, Ican Ilead Ito Iprejudicial Ibehavior, Isuch Ias Iproviders Itaking Imore Itime Iwith IWhiteIpatients Ithan IBlack Ipatients Iand Itherefore Ilearning Imore Iabout Ithe IWhite Ipatients’ Ineeds Iand Iconcerns. IAssess Iyour Icurrent Ilevel Iof Icultural Icompetence I(what Iknowledge, Iskills, Iand Iresources Ican Iyou Ibuild Ion? IWhere Iare Ithe Igaps?) IOne Ican Itake Ia Itest Ito Ilearn Imore Iabout Ione’s Iown Ibias. Healthcare is not a “one-size-fits-all” profession. It is important to be sensitive to ways in which culture and faith impact patients’ healthcare experiences. One good place to start with all patients is to let them know that you want to make them comfortable and ask them what they need. An attitude of openness and acceptance will do wonders. Demonstrating Iawareness Iof Ia Ipatient’s Iculture Ican Ipromote Itrust, Ibetter Ihealth Icare, Ilead Ito Ihigher Irates Iof Iacceptance Iof Idiagnoses Iand Iimprove Itreatment Iadherence. Health Iprofessionals Imay Iview Iclients Ior Ipatients Iwho Iare Iculturally Idifferent Ifrom Ithemselves Ias Iunintelligent Ior Iof Idiffering Iintelligence, Iirresponsible, Ior Idisinterested Iin Itheir Ihealth By Iassessing Icommunity, Iaggregate, Ifamily, Iand Iindividual Ifactors Iand Iconditions Ithat Ihave Ia Istrong Iinfluence Ion Ihealth, IAPRNs Iare Ibetter Iequipped Ito Ideliver Ieffective Iand Ievidence-based Icare. IIdentifying Ipopulation-level Ihealthcare Ineeds Iand Ihealthcare IdisparitiesIcan Ihelp Ito Iimprove Iequality Iin Ihealth Ioutcomes Iat Iall Ilevels. The IAPN Iwill Iassess Itheir Iown Iattitudes Iby Icultural Iawareness, Icultural Ihumility, Icultural Iknowledge, Icultural Iskill Iand Icultural Idesire. IWithout Ithis Ireflection Iand Ievaluation Iof Iour Iworld Icultural Ibeliefs Iand Ipractices, Ithe Inurse Iwill Ibe Iinfluenced Isubconsciously. Cultural IAwareness Self-examination Iof Ione's Iown Iprejudices Iand Ibiases Itoward Iother Icultures. IAn Iin-depth Iexploration Iof Ione's Iown Icultural/ethnicIbackground. Cultural IHumility A Ilifelong Icommitment Ito Iself-evaluation Iand Iself-critiques, Iredressing Ithe Ipower Iof Iimbalances Iin Ithe Ipatient- Iphysician Idynamic, Ideveloping Imutually. IBeneficial Irelationships.