HFMA CRCR EXAM LATEST 2025-2026 EXAM 170+ QUESTIONS AND CORRECT ANSWERS (VERIFIED ANSWERS)
Course:
HFMA CRCR
Institution:
HFMA CRCR
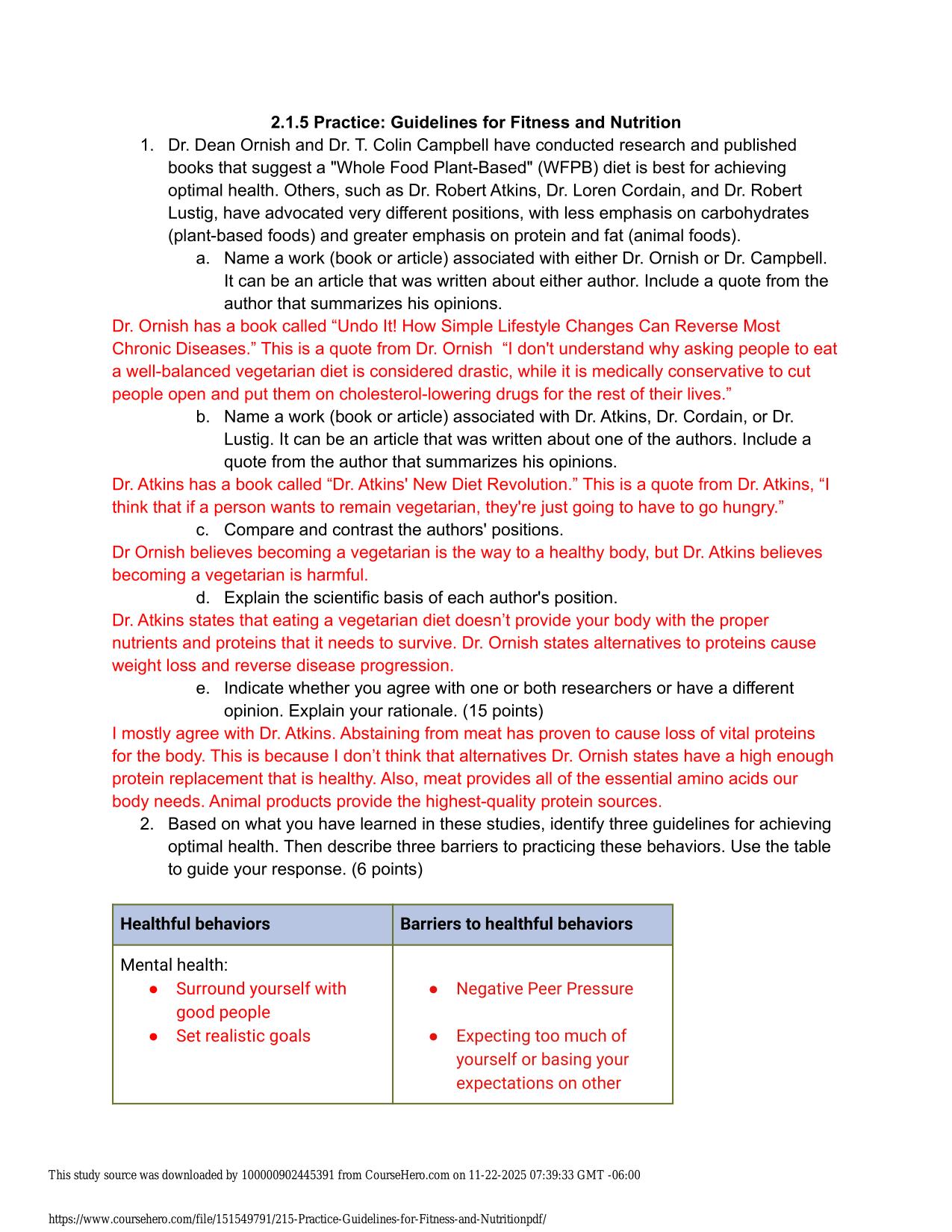
HFMA CRCR EXAM LATEST 2025-2026 EXAM 170+ QUESTIONS AND CORRECT ANSWERS (VERIFIED ANSWERS) IF outpatient diagnostic services are provided within three days of the admission of a Medicare beneficiary to an IPPS (Inpatient Prospective Payment System) h...
After purchase, you get:
✅ Instant PDF Download
✅ Verified answer explanations
✅ Refund if not Satisfied
✅ Prepared for 2025/2026 test cycle
Overview
Questions are arranged to build from basic concepts to more advanced challenges, making the learning curve smoother and more systematic. You'll notice your self-assurance growing naturally as you learn thoroughly each level before moving to the next. This scaffolding approach prevents that overwhelmed feeling that often comes with jumping into complex topics too quickly. Many learners appreciate how this progression mirrors the way we naturally learn - building step by step from simple to sophisticated.
Who Is This For?
Built for independent learners, study groups, and classroom instructors who require reliable exam-prep content in HFMA CRCR. Teachers often incorporate these materials into their lesson plans. The consistent quality makes it a trusted resource semester after semester.
Related Keywords
Detailed Study Description
Frequently Asked Questions
Document Information
| Uploaded on: | November 1, 2025 |
| Last updated: | November 17, 2025 |
| Number of pages: | 20 |
| Written in: | 2025/2026 |
| Type: | Exam (elaborations) |
| Contains: | Questions & Answers |
| Tags: | HFMA CRCR EXAM LATEST 2025-2026 EXAM 170+ QUESTIONS AND CORRECT ANSWERS (VERIFIED ANSWERS) IF outpatient diagnostic services are provided within three days of the admission of a Medicare beneficiary to an IPPS (Inpatient Prospective Payment System) hospital, what must happen to these charges - ANSWER- They must be billed separately to the part B Carrier what is a recurring or series registration? - ANSWER- One registration record is created for multiple days of service What are nonemergency patients who come for service without prior notification to the provider called? - ANSWER- Unscheduled patients Which of the following statement apply to the observation patient type |
Seller Information
AdelineJean
User Reviews (0)
Exam (Elaborations)
$10.00
Add to Cart
100% satisfaction guarantee
Refund Upon dissatisfaction
Immediately available after purchase
Available in Both online and PDF
$10.00
| 0 sold
Discover More resources
Inside The Document
HFMA CRCR EXAM LATEST 2024-2025 EXAM 170+ QUESTIONS AND CORRECT ANSWERS (VERIFIED ANSWERS) IF outpatient diagnostic services are provided within three days of the admission of a Medicare beneficiary to an IPPS (Inpatient Prospective Payment System) hospital, what must happen to these charges ANSWER- They must be billed separately to the part B Carrier what is a recurring or series registration? - ANSWER- One registration record is created for multiple days of service What are nonemergency patients who come for service without prior notification to the provider called? - ANSWER- Unscheduled patients Which of the following statement apply to the observation patient type? - ANSWER- It is used to evaluate the need for an inpatient admission which services are hospice programs required to provide around the clock patient - ANSWER- Physician, Nursing, Pharmacy Scheduler instructions are used to prompt the scheduler to do what? ANSWER- Complete the scheduling process correctly based on service requeste The Time needed to prepare the patient before service is the difference between the patients arrival time and which of the following? ANSWER- Procedure time Medicare guidelines require that when a test is ordered for a LCD or NCD exists, the information provided on the order must include: ANSWER- Documentation of the medical necessity for the test What is the advantage of a pre-registration program - ANSWER- It reduces processing times at the time of service What date are required to establish a new MPI(Master patient Index) entry - ANSWER- The responsible party's full legal name, date of birth, and social security number Which of the following statements is true about third-party payments? ANSWER- The payments are received by the provider from the payer responsible for reimbursing the provider for the patient's covered services. Which provision protects the patient from medical expenses that exceed the pre-set level - ANSWER- stop loss what documentation must a primary care physician send to HMO patient to authorize a visit to a specialist for additional testing or care? ANSWER- Referral Under EMTALA (Emergency Medical Treatment and Labor Act) regulations, the provider may not ask about a patient's insurance information if it would delay what? - ANSWER- Medical screening and stabilizing treatment Which of the following is a step in the discharge process? - ANSWERHave a case management service complete the discharge plan The hospital has a APC based contract for the payment of outpatient services. Total anticipated charges for the visit are $2,380. The approved APC payment rate is $780. Where will the patients benefit package be applied? - ANSWER- To the approved APC payment rate A patient has met the $200 individual deductible and $900 of the $1000 co-insurance responsibility. The co-insurance rate is 20%. The estimated insurance plan responsibility is $1975.00. What amount of coinsurance is due from the patient? - ANSWER- $100.00 When is a patient considered to be medically indigent? - ANSWER- The patient's outstanding medical bills exceed a defined dollar amount or percentage of assets. What patient assets are considered in the financial assistance application? - ANSWER- Sources of readily available funds , vehicles, campers, boats and saving accounts If the patient cannot agree to payment arrangements, What is the next option? - ANSWER- Warn the patient that unpaid accounts are placed with collection agencies for further processing What core financial activities are resolved within patient access? ANSWER- scheduling , pre-registration, insurance verification and managed care processing What is an unscheduled direct admission? - ANSWER- A patient who arrives at the hospital via ambulance for treatment in the emergency department When is it not appropriate to use observation status? - ANSWER- As a substitute for an inpatient admission Patients who require periodic skilled nursing or therapeutic care receive services from what type of program? - ANSWER- Home health agency Every patient who is new to the healthcare provider must be offered what? - ANSWER- A printed copy of the provider privacy notice Which of the following statements apples to self insured insurance plans? - ANSWER- The employer provides a traditional HMO health plan In addition to the member's identification number, what information is recorded in a 270 transaction - ANSWER- Name What process does a patient's health plan use to retroactively collect payments from liability automobile or worker's compensation plan? ANSWER- Subrogation In what type of payment methodology is a lump sum of bundled payment negotiated between the payer and some or all providers? ANSWER- DRG/Case rate What Restriction does a managed care plan place on locations that must be used if the plan is to pay for the service provided? - ANSWER- Site of service limitation Which of the following statements applies to private rooms? ANSWER- If the medical necessity for a private room is documented in the chart. The patients insurance will be billed for the differential Which of the following is true about screening a beneficiary of possible MSP(Medicare secondary payer) situations? - ANSWER- It is necessary to ask the patient each of the MSP questions Which of the following is not true of Medicare Advantage Plans? ANSWER- A patient must have both Medicare Part A and B benefits to be eligible for a Medicare Advantage plan Which of the following is a valid reason for a payer to deny a claim? ANSWER- Failure to complete authorization
CourseHero & Studypool Unlocks
Get Unlocked CourseHero and Studypool documents files instantly to your email, simply by pasting your link and clicking "Unlock Now". Learn more on how to unlock here.